Billy and I met in 1993 and married in 2002. He passed away in 2016.

Billy and I met in 1993 and married in 2002. He passed away in 2016.



Rocky and I met through another guy I was dating. It was a group of us hanging out together and when Rocky and I made eye contact, it was over for me. I broke up with my boyfriend, and later met Rocky in a rock and roll dive club. We exchanged numbers, but he didn’t call me quickly enough so I called him. We had our first date on April 8, 1983. I was 19 and he was 26. We were crazy for each other and always were. Our first kiss was as sweet as our last. He was diagnosed in July of 2017 and died on February 27th, 2019. Our life together was special. We couldn’t have children but it didn’t matter. He was my hero, my conscience, my soul mate, and best friend. I miss him more than I can bear.
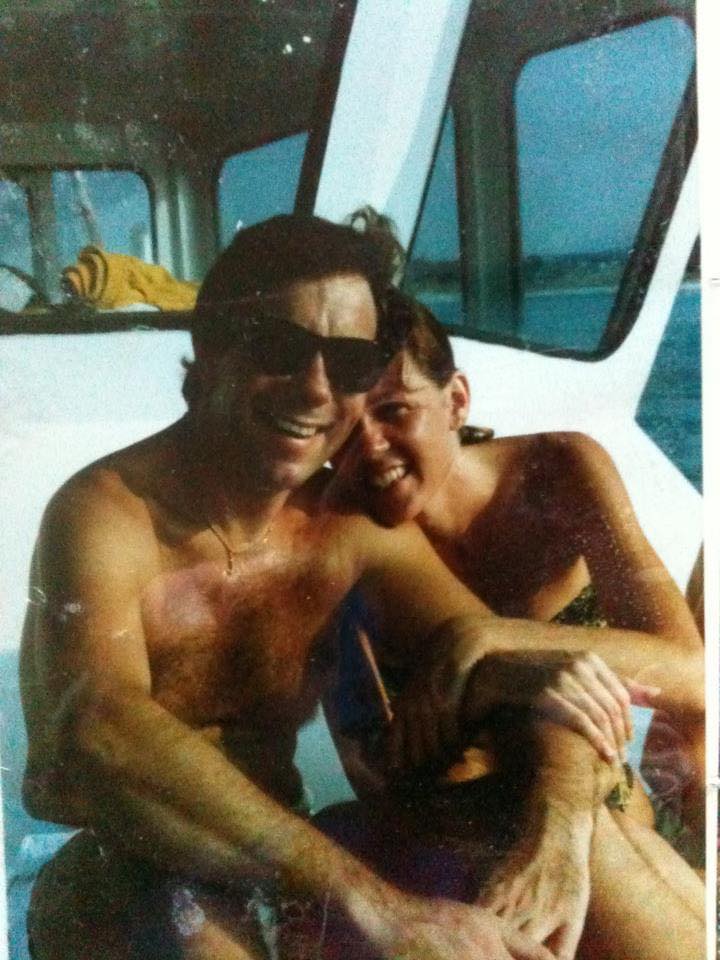
I was 17 when I met Steve. He was 27 and managing my brother’s best friends dive shop. I recall being introduced and him smiling and saying hello. He was so handsome, and English, and grown. I rarely spoke to him. Never in my wildest dreams did I think one day we would be married. Ten years later, after I had an extremely short marriage and nasty divorce, I moved back to the gulf coast. Steve and I reconnected and three months into dating married. We had a dream of a marriage, the kind everyone wishes for, the relationship my girlfriends all envied, the best thing ever. We had a well blended family, your mine and ours, with all loved equally. We were destined to be “that old couple”, together forever in love. But a nasty dragon entered our world in 2011, dragged my beautiful husband to a corner and slowly ate him alive in front of our very eyes. My Steve lived with stoic dignity with a smile always on his face while as we did our best for five years to beat that dam beast off of him. He walked through the dragon’s fire and shone as gold, an example to all he touched. His dragon was slain February 7 2016 and Steve went to his heavenly reward. We were married 26 years, not nearly long enough. I will live the rest of my days making him proud of me as I am of him. Love always wins
You often hear me reference ALS life versus real life. The reality is I’m living in both worlds. The “real” world involves chatting with Forrest, trying to decide what to have for dinner, managing the needs of the girls, changing sheets, playing games, spending time with friends/family and reading books. ALS life means helping Forrest manage his basic needs, scratching itches that can no longer be reached, being a voice that is no longer there or sometimes takes too long to articulate through his app. It means dressing changes, administering IV medication, catheter changes, refills of water, flushing picc lines, opening containers, adjusting clothes that have shifted and prepping medication.
ALS life also means thoughts about death are always on the periphery. Death is a constant companion when someone is diagnosed with ALS. You know that no one has ever been miraculously healed from ALS or gone into remission. You hear the statistic that the lifespan of someone with ALS is 3-5 years from onset and you wonder where your loved one will be on that spectrum. Or will you be lucky and your PALS (person with ALS) will go the Stephen Hawking route and defy all odds. Either way, your thoughts are never far from weighing those possibilities. Will it be quick and merciful? Will it be long but arduous? Or will you be lucky and find a peaceful middle place. Will we have time to prepare, will we get to say goodbye, will we have done everything we can to feel resolved?
I am in an online support group. It has been a lifeline for me since I found it. I have learned survival and adaptation skills in that group. They are in the trenches and collectively have more wisdom than a team of doctors could ever hope to have. We release our pain, vent frustrations, and share the gross/humorous/ridiculous realities of being a caregiver. It is simply amazing. But the realities of this disease are ever present. In a 24 hour period we had four PALS die not too long ago. There are currently 680 members in our group; many of those are people whose PALS have died but they have stayed in the group to offer their wisdom in support. Since January, over 40 of our PALS have died. Some of those were expected, and maybe even planned, and some were completely out of the blue. Some are peaceful and even joyful, and some are horrific and the stuff of nightmares. Some were less than a year after diagnosis. Some days it just feels like too much.
For our family, having someone who has ALS also means having hard conversations with our children and handling their hard questions and astute observations about death and dying. We have fully shared with them the realities of this disease. They know ALS is not something that goes away or that you recover from. They talk about missing his voice and ask when he might die and what that may be like. The last week of school Violette lovingly and so sweetly asked Forrest “you have the really bad ALS, don’t you?” Forrest nodded and gave her the thumbs up. She hugged him and as we were walking out to go to school she said, “mama if daddy dies while I’m at school, would you please get a note to my teacher?” The other day Sophie was talking about being an adult and made the comment that daddy wouldn’t be there. These are gut punching exchanges.
Some of the hardest conversations I have ever had are talking to my children about death and dying. But these are also some of my most proud conversations. When they talk about death as part of a bigger reality of our lives I know they are processing and reconciling that grief along the way and in a healthy way. They are sad, but they are honest and speak freely. And sometimes they start talking about TV or snacks two minutes after talking about death. We will all be devastated when that time comes, but they will not be blindsided by the reality.
ALS is so hard. And every day it gets harder. And shockingly we are no closer today to a cure or cause than we were 150 years ago, when it was first found, or 80 years ago when Lou Gerhig was diagnosed. You would think a disease that is considered most people’s worst case scenario would be farther along in research and the development of treatments.
We used an in-home care agency to provide caregivers for Mary so that I could continue to work, and to assist me with getting her up in the morning and to bed at night, tasks which needed two people. While one or two of the caregivers were amazing, I spent most of the time managing the agency staff and training them myself.
The in-home care agency nurse delegated multiple caregivers on medications and equipment who were not capable of administering medications or using the equipment. The nurse did not feel re-delegation was needed when equipment was updated, “as long as they read the manual”. She also made unscheduled visits that were upsetting to Mary, interfered with other appointments from home health therapists, and increased Mary’s anxiety.
One of the caregivers they sent was preaching her religious beliefs and had the same therapist as Mary. I fired her on day one.
Another caregiver became less confident each shift, was shaky and sweaty, and had to be constantly supervised. I fired her after one week.
One CNA caregiver was so nervous she dropped syringe of morphine on her first day. This was liquid morphine administered through Mary’s feeding tube, not an injection. I fired her on day two.
One caregiver failed to intervene with the transport driver while Mary was yelling “Stop! Stop!” Her wheelchair was not tied down correctly, causing her a neck injury which created multiple complications. The caregiver told the driver “You really hurt her”, but did not insist that the driver (an EMT) check her for injuries. Mary spent the next 2-3 days in bed with a migraine; the same caregiver spent her shifts at the other end of the house. Other caregivers spent their shifts in the room with Mary.
After a 4-hour training shift with an experienced caregiver/CNA, a new caregiver worked an evening shift, talking the entire time about how good he was, how he only has 12 hours a week off. It seemed this caregiver thought I – the wife – was another paid caregiver. He discussed which agencies were good to work for and which weren’t. He was reported to the agency out of concern for being overworked and thus a safety concern. I fired him after a week. He only got that much time because they had no one else to send.
The agency nurse came to the house to delegate another new male caregiver. She spent approximately 20 minutes at the house, and barely spoke to Mary. She told the new caregiver that Mary was on the feeding tube a couple of hours a day; Denise clarified that it was closer to 24 hours. Clearly the nurse was not current on Mary’s needs.
The same male caregiver did not appear to be comfortable caring for a female patient, and did not appear to have the ability to function in an emergency. Fired after a week.
A long-term caregiver was found to be padding her timesheet, not clocking out until after she had been gone. The same caregiver was late every morning, and discussed her friend’s x-rays with Mary’s home health team, monopolizing conversations rather than allow them to spend time with Mary. I fired her.
Two days later, Mary’s state-appointed case worker called to say the agency had given two-week’s notice and would terminate their care contract for Mary. A follow up call to the agency included multiple lies – the state-appointed case worker felt Mary should be in a facility, they just needed a “plan” within two weeks but would continue to provide care until the new plan was in place. The case worker called 30 minutes later saying that the agency manager had been very disrespectful to her on the phone and that she had the agency was the one who had said Mary should be in a facility. Pretty sure the agency lost state approval that day.
When the written notification arrived from the agency that the contract would be terminated, multiple reasons were given for the termination, stating that their nurse had stated she felt Mary should be in a nursing home, and that her insurance coverage did not cover two caregivers at the same time for transfers (untrue).
The last caregiver they sent before the contract terminated arrived sick. When questioned, he stated it was allergies, but the following day he called out sick. He had already infected Mary, who ended up in the ER with bronchitis, precipitating her decision to have a tracheotomy and be placed on a ventilator.
That was the end of our in-home care.
The agency’s website clearly stated that they were able to care for people with ALS, even until end of life. Yet the nurse had no experience with ALS, was not qualified to assess Mary’s needs, and clearly had no understanding of what appropriate facilities would be IF Mary would be placed in one. The agency repeatedly sent caregivers who were unqualified, untrained, and distracted by their phones. The caregivers were there so that I could continue to work, but I had to stay home many times to supervise them, defeating the purpose. Caregivers should have been instructed NOT to come if they were ill – they should not go to any patient’s home if they are ill.
I am forever grateful to one caregiver/CNA (now an RN) who DID have experience with ALS, who was compassionate, and who worked with us directly through the state during the brief time Mary was at home with the trach. She visited Mary in the hospital frequently, and they had a great relationship. Thank you MoGo.
Guest Post by Deborah Mast
Its ALS awareness month. ALS is 100% fatal. There are no cures and only one drug which may or may not extend life by a couple of months. I thought for a couple of days on how I want to seek awareness.
I decided that sharing the facts would be best and sharing that discrimination is not part of this fatal disease. It hits all ages, different ethnicities and can be passed down to several family members.
I have seen a young lady in her 20’s sitting at clinic instead of college, I have known young mothers, young fathers, a mother fighting ALS…who’s own son has been diagnosed. I know a women who has lost her mother, two brothers, two sisters and a aunt. I have watched small children say goodbye to one of their parents.
Although it usually strikes around age 55, doctors report that patients seem to be getting younger, for reasons they don’t understand. They’re increasingly encountering ALS patients in their twenties, thirties, even in their late teens.
I have known family members who may never recover from the battle with this grueling disease. I have known families who are financially devastated.
The facts are… there’s very little assistance for families with this disease, research is being done but yet the rates of ALS are continuing to climb and the ages are getting younger. I personally know the struggles this devastating disease causes.
The odds have increased. You will know someone with this disease. Can it be your family, your children, wife, husband, or friend? It did mine and I had no clue what this disease was.
You say what can I do? You can make awareness count buy sharing, by donating to research, by reaching out to those who are suffering and by signing laws into place to help these families and to help research. This is a disease that’s has spent a long time in the shadows just waiting for a break through.
Thank you for loving me enough to read this post.





Posted by permission of the author. One picture added to original post.
In the last 5 1/2 years, I have gained intimate awareness of ALS, so much so that it is now on my resume. Six years ago I would never have imagined that I would be comfortable changing the inner cannula of a trach, changing out a Mic-key button PEG tube, using an ambu bag, dialing 911 while frantically holding a face mask to my wife’s face to keep her breathing, making – literally – life and death decisions on an hourly basis. I would never have imagined the torture a body can experience, or imagined it would happen right in front of me over such a short period of time.
In the last 5 1/2 years, I have known hundreds of other spouses who cared for their partners through the devastation of ALS, and we have supported each other through our journeys while living with ALS and on the “other side” as we surviving spouses refer to it.
The ravages of ALS don’t end with the death of the person with ALS. They continue to haunt those of us on the other side, making it hard for us to trust anyone, to share what we experienced, because we spent so long hiding our vulnerability, keeping on a mask for our loved ones while crying and screaming in secret. While we lived with and tried to fight ALS, we didn’t share details with family members and friends – how could we? I didn’t want to burden my children, my parents, my friends with the fear, the anger, the horrors of what was required to care for my beloved, especially near the end. It is hard to imagine anyone understanding our journey except those who have also experienced it first-hand.
May is ALS Awareness Month. Again.

We are no closer to a cure, despite what you may hear and see out there.
Insurance companies are still denying medications, support services, equipment and in-home care services to people with ALS. How do you make someone with a terminal illness suffer even more? How do you not provide comfort care?
People are still choosing to bring their ALS journey to an end by refusing food and water, by removing their bi-pap and suffering for days, or by gunshot, because their states and/or providers will not ease their passing with common hospice-approved medications. The “opiod crisis” is creating horrible end-of-life experiences for those who have already been through so much. And their souses are left with severe PTSD (I do not use that term lightly), flashbacks and survivor’s guilt. As if we could possibly have done even more than we did.
ALS is not pretty. It is not a movie. It is not an easy thing to talk about. But we must talk about it, talk about the horrors, if we are ever to see funds supporting research to effectively diagnose, treat the symptoms, and one day find a cure.
And so I will be posting this month. I cannot guarantee it will be daily. I cannot guarantee it will be something I haven’t posted about before. Because even 5 1/2 years after my wife’s diagnosis, there are experiences and knowledge to share. Because even 3 1/2 years after my wife died, there are things that I need to say over and over again. Because I promised her that after she was gone, I would continue to fight for everyone else.
September 6, 2016
There is no time table for grief.
That whole “grieving for a year after losing a spouse” idea is bullshit. Each person walks through it differently. It can punch you in the gut just as intensely a year after the loss – or two – as it does the day of. And you never know what will trigger it.
Two weeks after the death, the support dries up and floats away like cremains. The surviving spouse becomes one of the walking dead, trying to rediscover who they are, trying to create who they want to become, all the while grieving the years of togetherness that were just torn away. The sleepless nights go on and on. Learning to cook for one person. Learning to go to the grocery store without them. Buying a car without them, or even a new TV. Painting the house.
You try to find friends who understand, who aren’t afraid of your “mood swings”, friends who and will try to guide you gently back into the world of the living. Finally, one day, you laugh about something and then you pick up your phone to call or text your spouse and tell them about it, and it hits all over again.You send your child off for their first day of kindergarten, of high school, of college, and no one understands why you are curled up in a ball. Your doctor tells you to get a colonoscopy and you have no one to drive you so you start crying, and the doctor tells you “we need to talk about your emotional health”, aka “you should be over this by now, we need to talk about meds.” You go to a family reunion and your spouse won’t be in the picture this time.
Just because someone’s Facebook page makes it look like they are doing ok, it doesn’t mean they are. It means they are doing the best they can, but most of the time it feels like they will never be ok again. It means they have stopped posting how they feel because they hear “you should be over this by now” or “have you talked to a therapist?” or they post and its crickets.
Grief is a roller coaster. Sometimes you just glide along, and then there is a 60 degree plummet and your stomach is in your throat. The difference is the plummet isn’t over in 60 seconds, and it takes a lot longer for the climb on the other side.
What can you do to help your friends and loved ones who are grieving? Let them know you are thinking about them. Let them know they are loved. Let them know that you don’t understand how they feel (unless you really do), but you will listen with an open heart. Let them take their time. Don’t push them to work through things because it makes you uncomfortable. Keep an eye on them in case they really do need professional help, but don’t assume they do just because they are still grieving 6 months, 12 months, 2 years later.
We will always grieve the loss. That doesn’t mean we are unhealthy. It means we loved deeply. We won’t show you most of the time just how bad it can be. We don’t want to burden you with it, and we don’t want to be told how to handle our emotions.
Just love us.
Also this week, In the middle of all of this, I called the ALS Clinic for a letter to trigger durable Power of Attorney. Mary is completely paralyzed and physically unable to manage her financial and legal affairs. Her facial muscles are also starting to have issues, so it is getting harder to read her lips when she mouths her words. The eye gaze device is still not working for her. The speech therapist who had been working with her had her hours cut to half-time and she has been unable to see her for nearly a month.
And Adult Foster Home #3, after three weeks of not returning phone calls, called the social worker late Wednesday and said they were “declining” Mary’s case because they didn’t realize she was on the vent 24/7, which is ridiculous because we told them that three weeks ago. Out of the nine homes in Oregon licensed to care for patients with ventilators, three have not worked out. She is still on the waiting list for the other 6. Now we wait for another bed to open up, and hope it is a reasonable distance. There is only one more option that is close to my route between work and home; the other five are anywhere from one to two hours away. Last week, Mary said that if this group home didn’t work out, she wants to wait for the next one, because she wants to have a chance to find out if she can find a way to communicate, which seems like it can’t happen until she is released from the hospital. I do have the number for the local sales rep for her eye gaze device; I plan to call her next week and see if she can come in and help us find something that will work.
While driving to see her after work, I got another call from the nurse. This time, it was because her pulse and blood pressure were elevated and the anti-anxiety medications hadn’t changed that. The doctor had ordered an EKG and they were going to go ahead and give her the same medication they had given her the last time. By the time I arrived, her pulse and bp had returned to normal rates and the EKG this time showed sinus tachycardia, which I was relieved to hear.
I put on my mask and spent a couple of hours (a bit longer than I had originally planned), making sure Mary was comfortable. I asked if she could tell the difference between this time and the last time and she said she could. We talked a little bit, talked to the nurses during shift change, then as she started to fall asleep I headed back home.
This is the second time there has been tachycardia and IV medications involved to resolve it. I am concerned that this lowers her chances of adult foster home placement even more.