You often hear me reference ALS life versus real life. The reality is I’m living in both worlds. The “real” world involves chatting with Forrest, trying to decide what to have for dinner, managing the needs of the girls, changing sheets, playing games, spending time with friends/family and reading books. ALS life means helping Forrest manage his basic needs, scratching itches that can no longer be reached, being a voice that is no longer there or sometimes takes too long to articulate through his app. It means dressing changes, administering IV medication, catheter changes, refills of water, flushing picc lines, opening containers, adjusting clothes that have shifted and prepping medication.
ALS life also means thoughts about death are always on the periphery. Death is a constant companion when someone is diagnosed with ALS. You know that no one has ever been miraculously healed from ALS or gone into remission. You hear the statistic that the lifespan of someone with ALS is 3-5 years from onset and you wonder where your loved one will be on that spectrum. Or will you be lucky and your PALS (person with ALS) will go the Stephen Hawking route and defy all odds. Either way, your thoughts are never far from weighing those possibilities. Will it be quick and merciful? Will it be long but arduous? Or will you be lucky and find a peaceful middle place. Will we have time to prepare, will we get to say goodbye, will we have done everything we can to feel resolved?
I am in an online support group. It has been a lifeline for me since I found it. I have learned survival and adaptation skills in that group. They are in the trenches and collectively have more wisdom than a team of doctors could ever hope to have. We release our pain, vent frustrations, and share the gross/humorous/ridiculous realities of being a caregiver. It is simply amazing. But the realities of this disease are ever present. In a 24 hour period we had four PALS die not too long ago. There are currently 680 members in our group; many of those are people whose PALS have died but they have stayed in the group to offer their wisdom in support. Since January, over 40 of our PALS have died. Some of those were expected, and maybe even planned, and some were completely out of the blue. Some are peaceful and even joyful, and some are horrific and the stuff of nightmares. Some were less than a year after diagnosis. Some days it just feels like too much.
For our family, having someone who has ALS also means having hard conversations with our children and handling their hard questions and astute observations about death and dying. We have fully shared with them the realities of this disease. They know ALS is not something that goes away or that you recover from. They talk about missing his voice and ask when he might die and what that may be like. The last week of school Violette lovingly and so sweetly asked Forrest “you have the really bad ALS, don’t you?” Forrest nodded and gave her the thumbs up. She hugged him and as we were walking out to go to school she said, “mama if daddy dies while I’m at school, would you please get a note to my teacher?” The other day Sophie was talking about being an adult and made the comment that daddy wouldn’t be there. These are gut punching exchanges.
Some of the hardest conversations I have ever had are talking to my children about death and dying. But these are also some of my most proud conversations. When they talk about death as part of a bigger reality of our lives I know they are processing and reconciling that grief along the way and in a healthy way. They are sad, but they are honest and speak freely. And sometimes they start talking about TV or snacks two minutes after talking about death. We will all be devastated when that time comes, but they will not be blindsided by the reality.
ALS is so hard. And every day it gets harder. And shockingly we are no closer today to a cure or cause than we were 150 years ago, when it was first found, or 80 years ago when Lou Gerhig was diagnosed. You would think a disease that is considered most people’s worst case scenario would be farther along in research and the development of treatments.




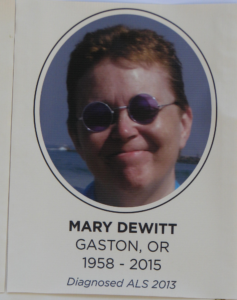 een 19 months since Mary crossed to the Summerlands. I promised her that when she was done fighting, I would fight for everyone else. This months’ posts have been one way I continue to do that.
een 19 months since Mary crossed to the Summerlands. I promised her that when she was done fighting, I would fight for everyone else. This months’ posts have been one way I continue to do that. spoken to in a while, and hear her “nasally” voice and ask if she was ok. “Oh, it’s just a cold. I’m fine.” Those were the ones she didn’t tell about the ALS. Others would call and ask how she was doing. “I’m doing GREAT!” she
spoken to in a while, and hear her “nasally” voice and ask if she was ok. “Oh, it’s just a cold. I’m fine.” Those were the ones she didn’t tell about the ALS. Others would call and ask how she was doing. “I’m doing GREAT!” she 


